Difference between revisions of "IPS implementationguide 2"
| Line 30: | Line 30: | ||
}} | }} | ||
| − | |||
{{:IN2}} | {{:IN2}} | ||
{{:IT2}} | {{:IT2}} | ||
| Line 41: | Line 40: | ||
{{:CF2}} | {{:CF2}} | ||
{{:AX2}} | {{:AX2}} | ||
| − | |||
[[Category:IG]] | [[Category:IG]] | ||
Revision as of 13:56, 6 August 2024
Continuous Build
This is the Continuous Build of the HL7 CDA® R2 Implementation Guide International Patient Summary (will be incorrect/inconsistent at times).
See the Directory of the published standard.
This document contains: Standard for Trial Use International Patient Summary (2.00). The text materials belong to category cdaips.
International Patient Summary
STU Release 2 (Universal Realm)
© 2024 Health Level Seven International ® ALL RIGHTS RESERVED. The reproduction of this material in any form is strictly forbidden without the written permission of the publisher. HL7 and Health Level Seven are registered trademarks of Health Level Seven International. Reg. U.S. Pat & TM Off.
Use of this material is governed by HL7's IP Compliance Policy.
| Role | Name | Organization | Contact |
|---|---|---|---|
| Primary Editor | Giorgio Cangioli | Consultant, HL7 Italy | giorgio.cangioli@gmail.com |
| Primary Editor | Rob Hausam | Hausam Consulting LLC | rob@hausamconsulting.com |
| Primary Editor | Dr Kai U. Heitmann | Heitmann Consulting and Services, ART-DECOR Open Tools GmbH, HL7 Germany | info@kheitmann.de |
| Primary Editor | François Macary | Phast | francois.macary@phast.fr |
| Contributor | Dr Philip Scott | HL7 UK | philip.scott@uwtsd.ac.uk |
| Contributor | Dr Christof Geßner | HL7 Germany | christof.gessner@mxdx.de |
| Contributor | Dr Stefan Sabutsch | ELGA, HL7 Austria | stefan.sabutsch@elga.gv.at |
| Contributor | Gary Dickinson | CentriHealth | gary.dickinson@ehr-standards.com |
| Contributor | Catherine Chronaki | HL7 International Foundation | chronaki@gmail.com |
| Contributor | Dr Stephen Chu | HL7 Australia | chuscmi88@gmail.com |
| Contributor | Didi Davis | The Sequoia Project | ddavis@sequoiaproject.org |
| Contributor | George Dixon | Allscripts LLC | george.dixon@allscripts.com |
| Contributor | Kenneth Sinn | Ontario Health Digital Services | ken.sinn@ontariohealth.ca |
| Contributor | John D'Amore | More Informatics | johnd@moreinformatics.com |
Thanks to Alexander Berler (a.berler@gnomon.com.gr); Carina Seerainer (carina.seerainer@elga.gv.at); John Roberts (John.A.Roberts@tn.gov); Julie James (julie_james@bluewaveinformatics.co.uk); Mark Shafarman (mark.shafarman@earthlink.net); Fernando Portilla (fportila@gmail.com); Ed Hammond (william.hammond@duke.edu); Steve Kay (s.kay@histandards.net).
Introduction
An International Patient Summary (IPS) document is an electronic health record extract containing essential healthcare information about a subject of care. As specified in EN ISO 27269, it is designed for supporting the use case scenario for ‘unplanned, cross border care’, but it is not limited to it. It is intended to be international, i.e., to provide generic solutions for global application beyond a particular region or country.
The IPS dataset is minimal and non-exhaustive; specialty-agnostic and condition-independent; but still clinically relevant.
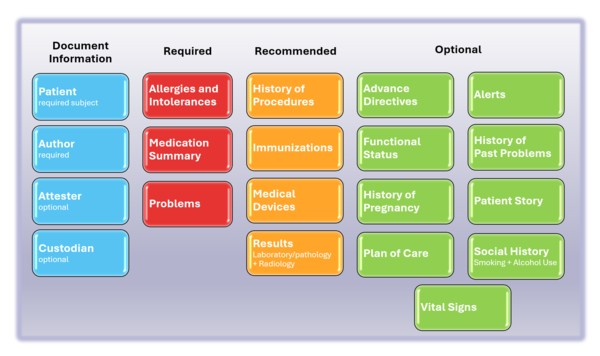
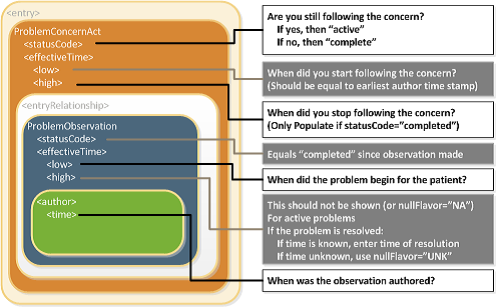
The IPS document is composed by a set of robust, well-defined and potentially reusable sets of core data items (indicated as IPS library in the figure below). The tight focus of the IPS on unplanned care is in this case not a limitation, but, on the contrary, facilitates their potential re-use beyond the IPS scope.
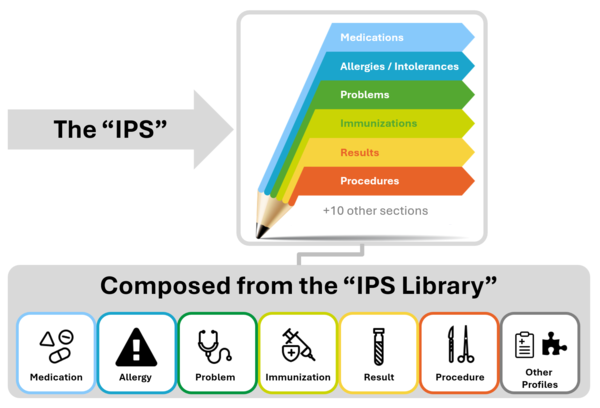
Figure 1: The IPS product and by-products
Purpose
The goal of this Implementation Guide is to specify how to represent in HL7 CDA the International Patient Summary (IPS). An alternative representation as templated HL7 FHIR R2 is also provided ( see the hl7.org site ). The initial focus of the International Patient Summary (IPS) was the unplanned care across national borders. This specification can be used and be useful also in local applications and be supportive of planned care.
Scope
As specified in EN ISO 27269, the IPS dataset is a “minimal, non-exhaustive set of data elements required for the international patient summary”. A Patient Summary is defined by ISO/TR 12773-1:2009 as a “Health record extract comprising a standardized collection of clinical and contextual information (retrospective, concurrent, prospective) that provides a snapshot in time of a subject of care’s health information and healthcare.”
‘Minimal’ reflects the ideas of ‘summary’ and the need to be concise, but also alludes to the existence of a core set of data elements that all health care professionals can use; it is intended to be a specialty agnostic and condition independent set. It does not imply that all the items in the data set will be used in every summary. It is also possible to refine the extract from a record such that the content of the summary is more relevant to a particular condition (e.g. asthma) but no asthma-specific elements will be specified in this standard. The IPS Document or IPS can be extended by non-IPS standard condition-specific data. ‘Non-exhaustive’ recognizes that the ideal data set is not closed, and is likely to be extended, not just in terms of requirement evolution, but also pragmatically in instances of use. [EN ISO 27269].
Furthermore the scope of the IPS is global. Although this is a major challenge, this implementation guide takes various experiences and newer developments into account to address, as far as possible, global feasibility.
The following picture provides an overview of the current IPS content.
Project Background and relationships with other projects
Details on the project background and relationships with other projects are available in the IPS Website.
Ballot Status of the Document
This Implementation Guide is STU with the intention to go normative.
Audience
The audience for this Implementation Guide includes:
Public
- Citizens who want to carry or access their healthcare data for emergency or unplanned care purposes.
Regulatory
- Policy makers such as healthcare payers or government agencies.
- Healthcare information governance authorities and regulatory bodies.
Clinical
- Healthcare providers that offer unscheduled and emergency care.
- Healthcare providers that populate regional and national patient summaries.
Technical
- Vendors of EHR systems for unplanned care management, personal health records and mobile health data applications.
- System integrators.
- Organizations that manage regional and national patient summaries.
Reading Publication Artifacts
A reading guide is available that explains the formalism used to express the publication artifacts, i.e. template meta data and template design. For convenience the guide is included in the appendix. (see section "How to read the table view for templates")
Technical Background
What is a CDA
CDA R2 is
… a document markup standard that specifies the structure and semantics of clinical documents for the purpose of exchange.
[CDA R2 Standard http://www.hl7.org/implement/standards/product_brief.cfm?product_id=7, Section 1.1]
Clinical documents, according to CDA, have the following characteristics:
- Persistence
- Stewardship
- Potential for authentication
- Context
- Wholeness
- Human readability
CDA defines a header for classification and management and a document body that carries the clinical record. While the header metadata are prescriptive and designed for consistency across all instances, the body is highly generic, leaving the designation of semantic requirements to implementation.
Templated CDA
CDA R2 can be constrained by mechanisms defined in the “Refinement and Localization” section of the HL7 Version 3 Interoperability Standards. The mechanism most commonly used to constrain CDA is referred to as “templated CDA”. This specification created a set of artifacts containing modular CDA templates (and associated value sets) for the purpose of the International Patient Summary, and the templates can be reused across any number of CDA document types.
There are different kinds of templates that might be created. Among them, the most common ones are:
- CDA Document Level Templates constrain fields in the Clinical Document Architecture (CDA) header, and define containment relationships to CDA sections.
For example, a History-and-Physical document-level template might require that the patient’s name be present, and that the document contain a Physical Exam section. - CDA Header Level Templates constrain fields for parts of the CDA header, like the patient (record target), the author, participations or the service event.
-
CDA Section Level Templates constrain fields in the CDA section, and define containment relationships to CDA entries.
For example, a Physical-exam section-level template might require that the section/code be fixed to a particular LOINC code, and that the section contain a Systolic Blood Pressure observation. -
CDA Entry Level Templates constrain the CDA clinical statement model in accordance with real world observations and acts.
For example, a Systolic-blood-pressure entry-level template defines how the CDA Observation class is constrained (how to populate observation/code, how to populate observation/value, etc.) to represent the notion of a systolic blood pressure.
Open and Closed Templates
Open templates permit anything to be done in the underlying standard that is not explicitly prohibited. This allows templates to be built up over time that extend and go beyond the original use cases for which they were originally designed.
Closed templates only permit what has been defined in the template, and do not permit anything beyond that. There are good reasons to use closed templates, sometimes having to do with local policy. For example, in communicating information from a healthcare provider to an insurance company, some information may need to be omitted to ensure patient privacy laws are followed. Most templates developed for CDA are of the open sort.
Template versioning
Template versioning is needed to enable template designs to evolve over time.
Template versioning enables template designers to control and shape the conformance statements that make up a template’s design over time tailoring the design to fit the template’s intended purpose.
Each template version is associated with a particular template. The template – as a whole – has a mandatory globally unique, non-semantic, identifier. The identifier serves as the identifier of the original intent of the template and as the identifier of the set of versions that represent the template over time.
Template versions have a mandatory timestamp (date and optional time), called the “effective date”. The date can be seen as the point in time when the template version “came into being”, i.e. was recognized as existent by the governance group. Use of the template prior to this date would be considered an invalid use of the template.
For further information on Templates, Template Versions and related topics refer to the HL7 Templates Standard [HL7 Templates Standard: Specification and Use of Reusable Information Constraint Templates, Release 1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=377].
Conformance Verbs
The conformance verb keywords SHALL, SHOULD, MAY and SHALL NOT in this document are to be interpreted as described in the HL7 Version 3 Publishing Facilitator's Guide [HL7 Version 3 Publishing Facilitator's Guide http://www.hl7.org/v3ballot/html/help/pfg/pfg.htm].
- SHALL: an absolute requirement
- SHALL NOT: an absolute prohibition against inclusion
- SHOULD: best practice or recommendation. There may be valid reasons to ignore an item, but the full implications must be understood and carefully weighed before choosing a different course
- MAY: truly optional; can be included or omitted as the author decides with no implications
Identifiers for Templates and Value Sets
This specification uses the following OIDs for the artifacts that are registered at the HL7 OID registry.
-
The root OID for templates is 2.16.840.1.113883.10.22
- Document Level Templates are sub branch .1, e.g. 2.16.840.1.113883.10.22.1.2 International Patient Summary
- Header Level Templates are summarized under 2.16.840.1.113883.10.22.2, e.g. 2.16.840.1.113883.10.22.2.1 IPS CDA recordTarget
- Section Level Templates are summarized under 2.16.840.1.113883.10.22.3, e.g. 2.16.840.1.113883.10.22.3.1 IPS Medication Summary Section
- Entry Level templates are summarized under 2.16.840.1.113883.10.22.4, e.g. 2.16.840.1.113883.10.22.4.19 IPS Certainty Observation
- “other” assistance templates are summarized under 2.16.840.1.113883.10.22.9, e.g. 2.16.840.1.113883.10.22.9.2 IPS CDA Device
- The root OID for Value Sets is 2.16.840.1.113883.11
The sub branches for templates follow the recommendations of HL7 International and ISO 13582 [ISO/TS 13582:2015 Health informatics -- Sharing of OID registry information]
Terminologies
Note: Much of the description provided in this section is copied and adapted from the §4.2.8 Vocabulary Conformance section of the C-CDA DSTU R2.1 Implementation Guide Volume 1 [HL7 C-CDA Implementation Guide DSTU R2.1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=379 ]
The templates in this document use terms from several code systems. These vocabularies are defined in various supporting specifications and may be maintained by other bodies, as is the case for the LOINC® and SNOMED CT® vocabularies. The primary terminologies identified for this specification are listed in the Design conventions and principles, section "How to use terminologies (preferred binding)".
Note that value set identifiers (e.g., ValueSet 2.16.840.1.113883.1.11.78 Observation Interpretation (DYNAMIC)) used in the binding definitions of template conformance statements do not appear in the XML instance of a CDA document. The definition of the template must be referenced to determine or validate the vocabulary conformance requirements of the template.
Value set bindings adhere to HL7 Vocabulary Working Group best practices, and include both an indication of stability and of coding strength for the binding. Value set bindings can be STATIC, meaning that they bind to a specified version of a value set, or DYNAMIC, meaning that they bind to the most current version of the value set. If a STATIC binding is specified, a date SHALL be included to indicate the value set version. If a DYNAMIC binding is specified, the value set authority and link to the base definition of the value set SHALL be included, if available, so implementers can access the current version of the value set. When a vocabulary binding binds to a single code, the stability of the binding is implicitly STATIC.
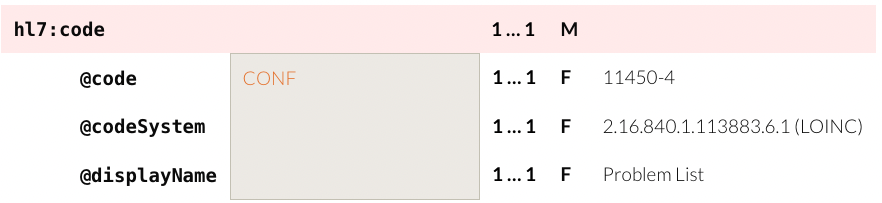
For example, to convey @code=11450-4, the code’s displayName 'Problem List', the OID of the codeSystem from which the code is drawn '2.16.840.1.113883.6.1', and the codeSystemName 'LOINC', the tabular view used in this guide is presented as shown below.
Figure: Binding to a Single Code (tabular view)
HL7 Data Types Release 1 requires the codeSystem attribute unless the underlying data type is “Coded Simple” or “CS”, in which case it is prohibited. The displayName and the codeSystemName are optional, but recommended, in all cases.
The above example would be properly expressed as follows.
<code code="11450-4" codeSystem="2.16.840.1.113883.6.1"/>
<!-- or -->
<code code="11450-4" codeSystem="2.16.840.1.113883.6.1" displayName="Problem List" codeSystemName=”LOINC”/>Figure: XML Expression of a Single-Code Binding
A full discussion of the representation of vocabulary is outside the scope of this document; for more information, see the HL7 V3 Normative Edition 2010 [HL7 V3 Normative Edition 2010 http://www.hl7.org/memonly/downloads/v3edition.cfm] sections on Abstract Data Types and XML Data Types R1.
There is a discrepancy between the HL7 R1 Data Types and this guide in the implementation of translation code versus the original code. The R1 data type requires the original code in the root. The convention agreed upon for this implementation guide is that a code from the required value set is used in the element and other codes not included in the value set are to be represented in a translation for the element. Note: This discrepancy is resolved in HL7 Data Types R2, but that is not available for use in CDA R2.
In the next example, the conformant code is SNOMED CT code 206525008.
<code code="206525008" codeSystem="2.16.840.1.113883.6.96"
displayName="neonatal necrotizing enterocolitis" codeSystemName="SNOMED CT">
<translation code="NEC-1" codeSystem="2.16.840.1.113883.19"
displayName="necrotizing enterocolitis"/>
</code>
Figure: Translation Code Example
Value set tables are present below a template, or are referenced if they occur elsewhere in the specification, when there are value set bindings in the template. The value set table provides the value set identifier, a description, and a link to the source of the value set when possible. Ellipses in the last row indicate the value set members shown are examples and the true source must be accessed to see all members.
If a value set binding has a DYNAMIC stability, implementers creating a CDA document must go to the location in the URL to check for the most current version of the value set expansion.
Note: Much of the description provided in the following three sections on value set definitions and expansions and extending value sets is adapted from Core Principles and Properties of HL7 Version 3 Models [Core Principles and Properties of HL7 Version 3 Models http://www.hl7.org/implement/standards/product_brief.cfm?product_id=58].
Value Set Definitions
Two approaches can be used to define the contents of a Value Set:
-
Extensional Definition: Explicitly enumerating each of the Value Set concepts.
- An Extensional Definition is an enumeration of all of the concepts within the Value Set. A Value Set defined by extension is composed of explicitly enumerated sets of concept representations (with the Code System in which they are valid). The simplest case is when the Value Set consists of only one concept.
-
Intensional Definition: Defining an algorithm that, when executed by a machine (or interpreted by a human being), yields an enumeration of all of the concepts within the Value Set, which is called a Value Set Expansion.
- An Intensional Definition is a set of rules that can be expanded (ideally computationally) to an exact set of concept representations at a particular point in time.
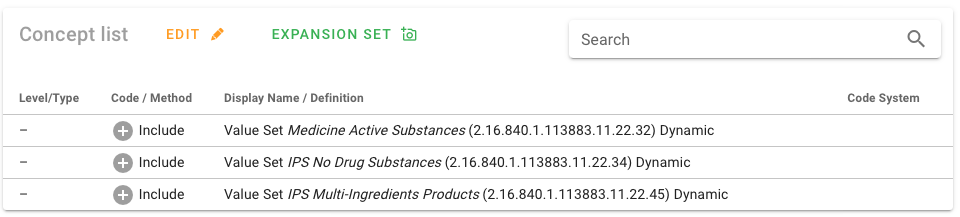
Many of the value sets used in the IPS specification are defined intensionally. The source of truth for these value sets and their definitions for IPS is ART-DECOR® [IPS Value Sets in ART-DECOR®].
Figure: Intensional value set definition.
Value Set Expansions
To obtain a list of enumerated concepts, Value Sets must be expanded. This means that the Value Set Definition must be converted to a list of concept representations at a point in time. This normally is a list of codes that may be used in populating or validating communicated model instances (but it may alternatively be a list of designations). While this is straightforward for extensional Value Set Definitions, an intensional Value Set Definition must be resolved to a Value Set Expansion by processing the rules contained in the Value Set Definition. Value Set Expansion can be done as early as the point of Value Set definition or as late as run time. For intensional Value Sets, the set of concepts contained in the expansion will generally change when the definition is changed (a new version of the Value Set Definition), but also may change with the identical version of the definition if the underlying code systems change, and the changes are part of the Value Set Expansion. This can be controlled if the definition statement refers to specific code system versions, thereby prohibiting the expansion from changing when the code system changes with a new version release. See Core Principles and Properties of HL7 Version 3 Models for additional details [Core Principles and Properties of HL7 Version 3 Models http://www.hl7.org/implement/standards/product_brief.cfm?product_id=58].
In order to implement the IPS specification, the intensionally defined value sets must be expanded (as noted above). ART-DECOR® provides capabilities for generating (and store) the required value set expansions. Other terminology servers are also expected to provide this service.
How to extend Value Sets
For elements with a binding to a value set that allows extensibility (Extensible/CWE), it may at times be necessary to extend the value set in order to support implementation needs. Coded With Extensibility (Extensible/CWE) means that the set of codes resulting from processing the Value Set Definition is not necessarily complete for its intended use-case. There may be some concepts that need to be communicated that cannot be represented within the expansion of the specified value set. In these cases, implementers therefore have permission to send local codes or original text within the coded element if an appropriate code cannot be found within the value set and its current expansion. When this does occur, however, there is an expectation that implementers should feed back these "missing concepts" to the maintainers of the Value Sets or referenced Code System(s) to have the necessary concept added, and then to transition to the new "official" code when one is subsequently added to the value set.
Functional requirements and high-level use cases
The International Patient Summary, i.e. a “specialty-agnostic, condition-independent" summary, was initially designed for cross-border unscheduled care, but its actual adoption is not limited to this usage scenario.
Patient summary initiatives are currently in various stages of development in different parts of the world. A summary of the most recent initiatives and experiences across the world can be found in the https://international-patient-summary.net/implementations-across-the-globe/.
As mentioned there are several options in terms of creation, sharing and usage of an IPS. For example:
- An IPS can be created when requested and used before, during, or after a care episode; or can be asynchronously generated and made available for future usage (e.g. store and retrieve).
- The IPS can be retrieved using a document exchange infrastructure; transported by the patient; or shared using cloud-services.
- The IPS may be subject of a transformation process that may include syntactical conversions, coded concept mappings and coded concept designation or free text translations. This transformation process may be performed in the creation phase, during the transmission, or after the IPS has been received, possibly using an external service.
- Finally, the received CDA may be used in different ways. For example, displayed using a common CDA stylesheet; display the extracted relevant information; incorporated into the receiver’s EHR. Alternatively, a specialized viewer may be adopted to enable the display of the translated content.
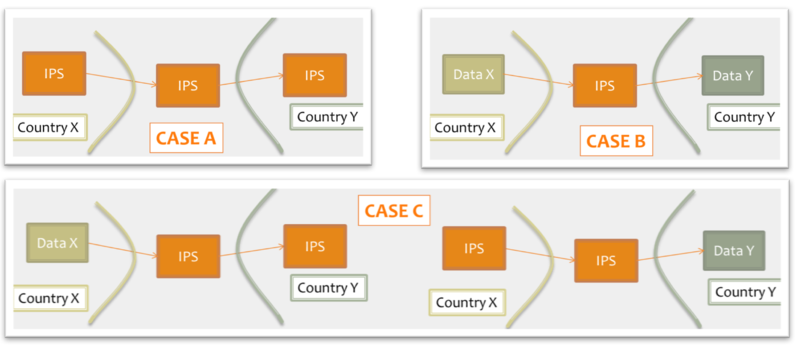
Moreover, for cross-jurisdiction exchange, the IPS could be used as:
- shared format among jurisdictions (case A), where jurisdictions originate and use IPS conforming documents unaltered.
- pivot document among existing summaries / data formats (case B). For example, the IPS is used as intermediate format between the US C-CDA CCD (please note that the CCD scope differs from that of the IPS) and the European eHDSI Patient Summary for a Transatlantic Patient Summary exchange.
- mixed mode (Case C), where either the originator or the consumer is expected to use an IPS conforming document.
Figure: Examples of IPS usage
An International Patient Summary may:
- be the result of automatic assembly (assembled IPS) or of a human summarization act (human curated IPS)
- have one or more EHR sources
- document information from a single or multiple jurisdictions/organizations
- aggregate input from a single or multiple encounters.
A clear determination of such contextual information raises the trustworthiness of the received IPS and helps the appropriate usage of its content by the receiver .
Most of these aspects are related to data provenance introduced in Chapter 5: Provenance.
Finally, there are several technical infrastructures and services that may be designed to support these requirements.
That said, it is out of scope of this standard to:
- give indications about solutions and strategies for the IPS creation, sharing, syntactical and semantic mapping, translation, and use.
- Provide guidance on how to determine the relevance of data for their inclusion in a IPS.
- Define selection or composition rules for facing potential inconsistencies from multiple sources in case of automatic collection.
- Impose constraints on the possible active Patient Summaries. Many jurisdictions require that only one active Patient Summary for unscheduled care is made available, but this is an implementation choice.
Code mappings and multilingual support
The capability of managing locally used coded concepts and reference terminologies, and that of providing receiving providers with human readable information in a language that can be understood by them, are critical aspects to be taken in account in the cross-border sharing of documents. This section summarizes some of the requirements related to these aspects, including also additional needs derived from the European cross-border services and some lessons learned by the EU/US Trillium Bridge Project.
The European cross-border services (Myhealth@EU), formerly known as eHDSI, use a business to business exchange infrastructure based on a network of country gateways that mediate access to the national infrastructures. The EU Patient Summary (EU PS) is used as a “pivot” document for the cross-border exchange. Local PS using data/document formats are in fact remapped into the eHDSI PS. The document exchanged is processed each time it passes through one of these gateway applying the needed syntactical transformation, code mappings. and translation of the code designations. Finally, in the current practice the received PSs are displayed using specialized display tools that build a human readable representation of the PS in the target language using the translated designations reported in the coded entries.
The adoption of translated narratives in the received document has been one of the indications received by the Trillium Bridge Project. This in fact allows extending multilingual support for the cross-border patient summaries to a wider set of potential consumers (EHR-or PHR systems), without requiring specialized viewers as applied in the eHDSI services.
Concept code mapping
In several real world use cases the records used as source for the Patient Summaries may use locally adopted terminologies, which are mapped to the reference value sets when possible, or otherwise used directly to provide uncoded information. This leads to a series of requirements listed below and detailed further in section "Design conventions and principles".
- When the original coded concept is mapped to one of the coded concepts included in the reference value sets (called hereafter reference code/coded concept), both the original and the reference codes SHALL be reported in the IPS instance.
- When the original coded concept is not mapped to one of the coded concepts included in the reference value sets, the original code SHALL be reported in the IPS instance as well as the indication that mapping was not successful.
- When the original record, for a specific coded element, is not able to provide coded but only textual information, this information SHALL be reported in the IPS instance.
This guide also accommodates these situations:
- The original record may support multi-coding. The IPS instance should make clear whether the additional codes belong to the original content or are the result of post hoc concept code mapping.
- The original record may include references to the pieces of text the coding was derived from. If present, the IPS instance should preserve this link between the original code and the referred text.
- Distinct original and reference coded concepts may belong to the same code system. This may be the result of a different level of granularity between the original and the reference value sets, or the result of format transformation - e.g. CCD document is used as input for generating an IPS. The requirement of recording both coded concepts applies also to these cases.
Multilingual support
Multilingual support by IPS can be split in two categories of action:
- The translation of coded concept designations (displayName)
- The translation of the narrative.
These actions may deal with various choices:
- Translation to the language of the receiving care provider: a foreign provider retrieves a translated copy of the IPS from the patient's country of affiliation…
- Translation to a commonly agreed language: an English version of the IPS is prepared.
- Predefined set of translations included in the shared IPS.
This guide does not favor any of these solutions. All of them are supported.
Translation of Designations
The European Cross-border services requires that for “safety and liability reasons” all of the original coded terms (designations, displayName) shall be recorded in the exchanged documents together with at least the English and the receiving country language terms (designations, displayName) associated with the reference codes. The designations translated in the receiving country language are used to generate the human readable content shown to the receiving provider. No free text translation is applied in this case. In order to accomplish this objective, the IPS should have the capability to record one or more designations, possibly indicating the language used. The solution chosen to fulfill this requirement is specified in section 4.6.
Narrative Translation
Narrative translation covers two kinds of operations:
- Translation of the original narrative text, which can be automated (e.g. using translation services) and/or human curated.
- Creation of new narrative for the target language, based on the coded entries.
The level of quality and liability obtained depends on the solution adopted and on the quality of the translation service used. It is out of the scope of this guide to suggest any of these solutions. In all cases, however:
- the language of the narrative should be identifiable
- the original and the translated narrative should be clearly distinguished
- the translation methodology applied (e.g. derived from the coded entries; translated by a generic service;..) should be noted
Design conventions and principles
How to use terminologies (preferred binding)
As stated in section 1.5, to be universally exchangeable the International Patient Summary must rely on international multilingual reference terminologies. To that effect, each codeable element of the international patient summary template is bound to a Value Set built upon an international reference terminology, such as SNOMED CT, LOINC, UCUM or EDQM Standard Terms. In some selected cases, in consideration of the availability of other globally usable reference terminologies and for alignment with a future FHIR version of the IPS, FHIR-defined terminologies have been specified. These terminologies have been selected to provide the preferred bindings for the codeable elements of the patient summary. They are the primary terminologies of this specification.
Nevertheless, it is anticipated that in some situations a system producing an instance of patient summary might not support one or the other of these primary terminologies, supporting only a local interface terminology instead. Similarly, it is also anticipated that the receiving system might in some cases not be able to use a code in a patient summary, either because this code belongs to a primary terminology that the receiving system does not support or because this code belongs to an interface terminology specific to the country of the producing system.
In order to maximize the international scope and usability of patient summaries, and also to accommodate the exceptional situations listed above, this specification makes these requirements:
- The Primary Code of a codeable element SHOULD be populated.
- If populated, the Primary Code of a codeable element SHALL be chosen from the primary terminology assigned to the value set bound to this element; unless exceptions have been agreed.
- The 'displayName' of the Primary Code SHALL be populated with a term representing this same code in the terminology used, in the language chosen for the current instance of the patient summary.
- When the primary 'code' element is not populated, an appropriate 'nullFlavor' value SHALL be used along with the 'originalText' element (referencing a textual expression in the narrative representing the meaning for the producer) and/or one or more coded 'translation' elements.
- One or more Alternate Codes from a local interface terminology MAY be provided, each with its associated 'displayName'.
- In case the primary code is derived from an alternate terminology the alternate code SHOULD be provided in the translation element.
Primary Code
In the data type for codeable elements (CD constrained by the CD.IPS template), the Primary Code is represented by the attributes @code, @displayName, @codeSystem, @codeSystemName, @codeSystemVersion.
Alternate Code
In the data type for codeable elements (CD constrained by the CD.IPS template), an Alternate Code is carried in a 'translation' sub-element.
Original Text
In the data type for codeable elements (CD constrained by the CD.IPS template), the Original Text is provided in the 'originalText' sub-element.
Representing "known absent" and "not known"
In line with the properties of minimalism and non-exhaustiveness for the IPS (see the IPS definition above), and benefiting from the experience acquired with the European cross-border services, this guide explicitly addresses two general situations:
- condition or activity unknown
- condition or activity known absent.
Other kinds of negations such as: (a) the negation of an allergy to a specific agent; (b) the absence of a particular disease; or (c) the fact that a specific vaccination has not been performed, have been considered beyond the set of essential data for an IPS.
This specification represents this core set of negations (“general condition/activity unknown” and “general condition/activity/known absent” ) using explicit coded elements rather than relying on specific mechanisms of HL7 CDA such as nullFlavor and negationInd attributes or human readable text (possibly not understood by the foreign country receiver).
In contrast to the practice to use negationInd or nullFlavor attributes on a section itself, we prohibit the use of these attributes on section level to express “unknown” or “no information” situations. A section holds the categorized (coded) narrative part of the documented activity and will never carry negationInd or nullFlavor attributes. Instead, we enforce by design, that “unknown” or “no information” expressions always go to the coded entry with a corresponding act code.
The main reasons for this choice are:
- @negationInd in CDA has been superseded in V3 later by two other negation indicators: @actNegationInd and @valueNegationInd.
- To make clinical content representation less dependent on a particular format or syntax, enabling a more practical path to transforming and exchanging data from one standard format (e.g. CDA R2) to another (e.g. FHIR).
- to provide one single method to express the presence or absence of a particular condition (e.g. an allergy) or activity (e.g. an immunization), or the lack of knowledge regarding this kind of condition or activity, resulting in a more robust and easily implementable specification.
For the other kinds of negations, not explicitly mentioned in this guide, it is suggested to apply – where possible – the same approach. Future versions of this guide may extend the number of cases covered and include new coded concepts for supporting them.
When needed, more specific statements such as the absence of a specific condition or activity, although considered as beyond the set of essential data for IPS, can still be expressed by using the native negationInd attribute of CDA R2.
Uncoded information
An IPS originator may not be able to value a coded element with an appropriate coded concept, but only with textual information. This may happen for two reasons:
- the originator is not able to express the concept in the reference value sets
- the originator is not able to express the concept in any known terminology.
The first case, assuming that the coding strength is Required (aka CNE, coded, no extensions), is represented in this guide with the following assertion:
<code codeSystem="2.16.840.1.113883.6.96" nullFlavor="OTH">
<originalText>
<reference value="#ref1"/>
</originalText>
</code>
That is expressing that there are no codes applicable in the referred code system (in the example, SNOMED CT). Please note that according to this guide the text is documented in the section narrative and only referenced by the coded element.
Note: Data Types R1 doesn't allow specifying that there are no codes applicable in the referred value set, as instead is possible with Data Types R2. Future versions of this guide may consider extending the data type to better support this situation.
The second case, that applies both to Required (aka CNE, coded no extensions) and Extensible (CWE, coded with extensions) coding strengths, is instead here represented valuing the coded element with the most generic nullFlavor “NI” (No Information) and pointing the text in the section narrative:
<value xsi:type="CD" nullFlavor="NI">
<originalText>
<reference value="#ref1"/>
</originalText>
</value>
Note: The most proper NullFlavor code to be used here would be "UNC" (Uncoded). This code is available in the current and other recent versions of the HL7 RIM, but it is not present in version 2.07 of the RIM on which the CDA R2 standard is based. In the absence of "UNC", the most appropriate NullFlavor code to use for representing that the data is unable to be coded is "NI".
Unmapped Coded Concepts
In several real world situations the records used as source for the Patient Summaries may use locally adopted terminologies mapped into the reference value sets. When the original coded concept cannot be mapped in one of the coded concepts included in the reference value sets, it is recommended to populate the original code in the IPS instance (in a 'translation' sub-element), with a nullFlavor indicating that the mapping didn’t occur. (See also the "Concept code mapping" in the section "Functional requirements and high-level use cases".). The nullFlavor value depends upon the coding strength of the binding.
Two circumstances are considered here: the case in which the coding strength is Required (CNE) and when it is Extensible (CWE).
In the case of coding strength Required (CNE), use nullFlavor "OTH":
<value xsi:type="CD" codeSystem="2.16.840.1.113883.6.96" nullFlavor="OTH">
[
<originalText>
<reference value="#ref1"/>
</originalText>
]
<translation code="A02.9" codeSystem="2.16.840.1.113883.6.3"
displayName="Infezioni da Salmonella non specificate"/>
</value>
The square brackets [ ] are used to indicate that the originalText element may or may not be present
Note: It may happen that a mapping would be possible in the target code system, but not in the target value set; Data Types R1 does not allow the specification of this difference, that there are no codes applicable in the reference value set, which is possible with Data Types R2.
Future versions of this guide may consider extending the data type to better support this situation.
In the case of Extensible (CWE) coding strength, this guide recommends representing the original code in the <translation> sub-element and using a nullFlavor for the primary code. This highlights the fact that a mapping to the reference value set was attempted, but no suitable target codes were identified.
<value xsi:type="CD" codeSystem="2.16.840.1.113883.6.96" nullFlavor="NI">
[
<originalText>
<reference value="#ref1"/>
</originalText>
]
<translation code="A02.9" codeSystem="2.16.840.1.113883.6.3"
displayName="Infezioni da Salmonella non specificate"/>
</value>
The square brackets [ ] are used to indicate that the originalText element may or may not be present.
Mapped coded concepts
As mentioned above, in several circumstances an original coded concept is mapped into the reference value set. When this occurs, both the original and the reference codes should be reported in the IPS instance.
Functional requirements exposed in "Concept Code Mapping" (multi-coding, link to original text, mapping between codes of the same code system) are also detailed below.
Case 1: Single local code mapped to primary code from the reference value set.
<value xsi:type="CD" code="42338000" codeSystem="2.16.840.1.113883.6.96"
displayName="Salmonella gastroenteritis">
[
<originalText>
<reference value="#ref1"/>
</originalText>
]
<translation code="003.0" codeSystem="2.16.840.1.113883.6.103"
displayName="Gastroenterite da Salmonella"/>
</value>
The square brackets [ ] are used to indicate that the originalText element may or may not be present
Case 2: Multiple local codes mapped together using nested 'translation' elements, and mapped to the primary code from the reference value set.
<value xsi:type="CD" code="422479008" codeSystem="2.16.840.1.113883.6.96"
codeSystemName="SNOMED CT"
displayName="FEMALE BREAST INFILTRATING DUCTAL CARCINOMA, STAGE 2">
[
<originalText>
<reference value="#problem4name"/>
</originalText>
]
<translation code="code-example" codeSystem="1.999.999"
codeSystemName="this is only an example"
displayName="FEMALE BREAST INFILTRATING DUCTAL CARCINOMA, STAGE 2">
<translation code="174.9" codeSystem="2.16.840.1.113883.6.103"
codeSystemName="ICD-9CM"
displayName="Malignant neoplasm of breast (female), unspecified"/>
<translation code="C50.919" codeSystem="2.16.840.1.113883.6.90"
codeSystemName="ICD-10-CM"
displayName="Malignant neoplasm of unspecified site of unspecified female breast"/>
</translation>
</value>
Case 3: Original and the reference coded concepts belong to the same code system (distinct codes). This may be the result of a different level of granularity between the original term and the reference value sets.
<code code="60591-5" codeSystem="2.16.840.1.113883.6.1"
codeSystemName="LOINC" displayName="Patient Summary">
<translation code="60592-3" codeSystem="2.16.840.1.113883.6.1"
displayName="Patient summary unexpected contact"/>
</code>
Note: The R1 data type definition identifies the <translation> as “a set of other concept descriptors that translate this concept descriptor into other code systems." There is however a common understanding that it may be more than one representation in a single code system where code systems allow multiple representations, such as SNOMED CT. Data Types R2 extended the possibility to provide translations also in the same code system.
Translation of designations
The capability of recording one or more designations, in different languages, for the exchanged Patent Summary is one of the functional requirements requested for “safety and liability reasons” by the European Cross-border services (see "Designations’ Translation" in section "Functional requirements and high-level use cases" for more details).
Given that the base CDA R2 standard which uses datatypes R1 does not offer a native way to convey the language translation of 'displayName', this guide introduces an optional 'ips:designation' extension to the CD datatype for that purpose.
Below are examples of usage of this extension.
No code mapping
<code code="60591-5" codeSystem="2.16.840.1.113883.6.1"
codeSystemName="LOINC" displayName="Patient Summary">
<ips:designation language="it-IT">Profilo Sanitario Sintetico</ips:designation>
<ips:designation language="fr-FR">Patient Summary</ips:designation>
<ips:designation language="en">Patient Summary</ips:designation>
</code>
Including code mapping
<value xsi:type="CD" code="42338000" codeSystem="2.16.840.1.113883.6.96"
displayName="Salmonella-gastroenterit">
<ips:designation language="da-DK">Salmonella-gastroenterit</ips:designation>
<ips:designation language="en">Salmonella gastroenteritis (disorder)</ips:designation>
[
<originalText>
<reference value="#ref1"/>
</originalText>
]
<translation code="003.0" codeSystem="2.16.840.1.113883.6.103"
displayName="Gastroenterite da Salmonella"/>
</value>
Narrative Translations
“Narrative translation” means both the translation of the original narrative text, that can be human curated or automatically performed, and the generation of a translated narrative based on the coded entries.
The functional requirements associated with this process are described in "Designations’ Translation" in section "Functional requirements and high-level use cases", and can be summarized in two main points : (a) language identification and (b) distinguishable original and translated narratives. Moreover, the methodology applied for the narrative translation (e.g. derived from the coded entries; translated by a generic service;..) should be noted.
Regarding the translation of section narrative <text>, this guide recommends providing this translation on purely textual subordinate sections (one per translation) as specified in the IPS Translation Section (2.16.840.1.113883.10.22.3.15) template.
An example of this is:
<section>
<templateId root="2.16.840.1.113883.3.1937.777.13.10.5"/>
<id root="..." extension="..."/>
<code code="48765-2" codeSystem="2.16.840.1.113883.6.1"
displayName="Allergies and adverse reactions"/>
<title>Allergies and Intolerances</title>
<text>No known Allergies</text>
<!-- omissions -->
<component>
<section>
<!-- subordinate section carrying a translation of the parent section -->
<title>Allergie ed Intolleranze</title>
<text>Nessuna Allergia Nota</text>
<languageCode code="it-IT"/>
</section>
</component>
</section>
Provenance
In the development of this Implementation Guide, consideration was given to the HL7 CDA® Release 2 Implementation Guide: Data Provenance, Release 1 - US Realm Draft Standard for Trial Use (December 2015). That guide provides a matrix offering a thorough and systematic analysis of provenance characteristics of electronic health records. Given the agreed scope principle (see section "Introduction") that the IPS be minimal and implementable, and the variable maturity and operational methods of existing national patient summaries, the proposal is that this first version should not attempt to require the full detail of that provenance specification.
The approach proposed for this version of the IPS is to:
- Allow optional documentation of section-level provenance.
- Require document-level provenance.
- Define IPS document provenance as one of two types: human-curated or software-assembled, based on the authors recorded in the header.
- The classification is based on whether the IPS document is constructed by a human or an automated process, regardless of whether the IPS contains some content of both kinds.
- Require the IPS source system to identify the IPS provenance type and author.
- The author shall be a human, if the IPS provenance type is "human-curated", or a device or system if the IPS provenance type is "software-assembled".
- In the case of a software-assembled IPS that is then verified by a human, the document provenance type shall be "software-assembled" and the author shall be the device or system that constructed the IPS document, but an additional verifier identity shall name the human who performed this check. For the avoidance of doubt, verifier is not the same as legalAuthenticator (the verifier is represented as a participant with typeCode "VRF"). However, in cases where the verifying person intentionally wishes to sign the document, this shall be recorded as a legalAuthenticator.
- Allow optional section level author, provenance type, verifier, and informant identification, for IPS source systems that can support this.
- Not attempt to implement the US Realm CDA data provenance templates.
Note: Discussions with the EHR work group suggest that a possible future project should be an IPS functional profile, once there is greater clarity and operational experience of using the IPS.
Representation of Names
This specification requires that any Person Name is represented including at least the given and family components and therefore is never documented as a single string.
Even though it is recognized that there is not in all cultures the same concept of “family name”, no evidence has been collected in analyzing the international context (e.g. Japan, Korea; China) that justifies the retirement of this requirement.
Moreover, due to the global scope of the International Patient Summary, the case of non-alphabetic representations of the names has also been considered.
In this case, to facilitate the global use of the IPS, at least one alphabetic representation of the name SHALL be provided.
Determining the Status of Clinical Statement
Note: Most of the description provided in this section is copied from the § 3.3 Determining the Status of Clinical Statement of the C-CDA DSTU R2.1 Implementation Guide Volume 1 [HL7 C-CDA Implementation Guide DSTU R2.1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=379].
A recipient must be able to determine whether the status of an entry — which can include a problem, a medication administration, etc. — is active, completed, or in some other state. Determination of the exact status is dependent on the interplay between an act’s various components (such as statusCode and effectiveTime). The following principles apply when representing or interpreting the status of a clinical statement.
- The Act.statusCode of the clinical statement specifies the state of the entry: Per the RIM, the statusCode “reflects the state of the activity. In the case of an Observation, this is the status of the activity of observing, not the status of what is being observed.”
- Act.statusCode and Act.moodCode are inter-related: Generally, an act in EVN (event) mood is a discrete event (a user looks, listens, measures, and records what was done or observed), so generally an act in EVN mood will have a statusCode of “completed.” A prolonged period of observation is an exception, in which a user would potentially have an observation in EVN mood that is “active.” For an Observation in RQO (request) mood, the statusCode generally remains “active” until the request is complete, at which time the statusCode changes to “completed.” For an Observation in GOL (goal) mood, the statusCode generally remains “active” as long as the observation in question is still an active goal for the patient.
- Act.statusCode and Act.effectiveTime are interrelated: Per the RIM, the effectiveTime, also referred to as the “biologically relevant time,” is the time at which the act holds for the patient. So, whereas the effectiveTime is the biologically relevant time, the statusCode is the state of the activity. For a provider seeing a patient in a clinic and observing a history of heart attack that occurred 5 years ago, the status of the observation is completed, and the effectiveTime is five years ago.
The IPS Problem Concern Entry and the IPS Allergy and Intolerance Concern templates reflect an ongoing concern on behalf of the provider that placed the concern (e.g. a disease, an allergy, or other conditions) on a patient’s problem or allergy list. The purpose of the concern act is that of supporting the tracking of a problem or a condition (e.g. an allergy). A concern act can contain one or more discrete observations related to this concern. Each of them reflects the change in the clinical understanding of a condition over time. For instance, a Concern may initially contain a symptom of “chest pain”, later identified as consequence of a gastroesophageal reflux. The later problem observation will have a more recent author time stamp.
There are different kinds of status that could be of clinical interest for a condition:
- The status of the concern (active, inactive,..)
- The status of the condition (e.g. active, inactive, resolved,..)
- The confirmation status [verification status, certainty] (e.g. confirmed, provisional, refuted,…)
Not all of them can be represented in a CDA using the statusCode elements of the concern (ACT) and observation (condition).
Status of the concern and related times
The statusCode of the Problem Concern Act is the definitive indication of the status of the concern. So long as the provider has an ongoing concern — meaning that the provider is monitoring the condition, whether it includes problems that have been resolved or not — the statusCode of the Concern Act is “active.” When the underlying conditions are no longer an active concern, the statusCode of the Problem Concern Act is set to “completed.”
The Concern Act effectiveTime reflects the time that the underlying condition was considered a concern. It may or may not correspond to the effectiveTime of the condition (e.g., even five years later, the clinician may remain concerned about a prior heart attack). The effectiveTime/low of the Concern Act asserts when the concern became active. This equates to the time the concern was authored in the patient's chart. (i.e. it should be equal to the earliest author time stamp) The effectiveTime/high asserts when the concern became inactive, and it is present if the statusCode of the concern act is "completed". If this date is not known, then effectiveTime/high will be present with a nullFlavor of "UNK".
Status of the condition and related times
Each Observation contained by a Concern Act is a discrete observation of a condition. Its statusCode is always “completed” since it is the “status of the activity of observing, not the status of what is being observed”. The clinical status of a condition (e.g. a disease, an allergy,..) is instead recorded by specialized subordinated observations (IPS Allergy Status Observation; IPS Problem Status Observation), documenting whether it is active, in remission, resolved, et cetera. The effectiveTime, also referred to as the "biologically relevant time", is the time at which the observation holds for the patient. For a provider seeing a patient in the clinic today, observing a history of penicillin allergy that developed six months ago, the effectiveTime is six months ago. The effectiveTime of the Observation gives an indication of whether or not the underlying condition is resolved, but the current status is documented by a subordinated observation. The effectiveTime/low (a.k.a. "onset date") asserts when the allergy/intolerance became biologically active. The effectiveTime/high (a.k.a. "resolution date") asserts when the allergy/intolerance was biologically resolved. If the date of resolution is not known, then effectiveTime/high will be present with a nullFlavor of "UNK".
Figure: Problem Concern Act (from C-CDA IG DTSU R2.1 HL7 C-CDA Implementation Guide DSTU R2.1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=379)
Confirmation status
The confirmation status, also noted as verification status or certainty, indicates the certainty associated with a condition (e.g. confirmed, provisional, refuted,…) providing information about the potential risk, for example, of a reaction to the identified substance. The confirmation status of a condition (e.g. a disease, an allergy,..) is recorded by a specialized subordinated observation (IPS certainty Observation), documenting whether the condition is confirmed, unconfirmed, provisional, refuted, et cetera.ge
The use of medication statements in the summary
A medication list may strongly vary depending on the context of use (e.g. support for prescription or dispensation, drug reconciliation, etc. ) and on the type of information reported (e.g. patient-reported medication, prescribed, dispensed or administered medications, active or past medications, etc.).
This is still true also for the medication summary in a Patient Summary. It could be, for instance, a list of "Relevant prescribed medicines whose period of time indicated for the treatment has not yet expired whether it has been dispensed or not, or medicines that influence current health status or are relevant to a clinical decision " (European eHN Guideline on the electronic exchange of health data under Cross-Border Directive 2011/24/EU: Patient Summary. Release 3.3.; a list of actually dispensed medications; a list of relevant medications for the patient (IHE PCC, IHE Patient Care Coordination Technical Framework http://ihe.net/Technical_Frameworks/#pcc); or conversely, it could be a complete history including the full patient's prescription and dispensation history and information about intended drug monitoring (C-CDA [HL7 C-CDA Implementation Guide DSTU R2.1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=379]).
Moreover, for the scope of the International Patient Summary, it is important to know what medications are being taken by or have been given to a patient; without necessarily providing all the details about the medication order, supply, administration or monitoring. This information need, in line with the IPS principle of minimum non exhaustive data, is well expressed by the concept of Medication Statement (see https://www.hl7.org/fhir/medicationstatement.html). The IPS medication summary is therefore typically a list of relevant medication statements, possibly built from either a prescription list or a dispensation list. In fact, in many practical cases data included in a Patient Summary are derived from the list of the medicines prescribed by a GP and recorded in its EHR-S; or extracted from a regional/national prescribing and/or dispensation systems. In these cases, data obtained from actual dispensation and/or prescription records can be still recorded in the IPS as statements and the original request, supply or administration records referred by the statement if really needed.
Medicinal Product Identification
The identification of medicinal products is quite easily solved within a single jurisdiction relying on local drug databases. In contrast, it is one of the major open issues for eHealth services across jurisdictions.
The set of ISO standards called IDMP [IDMP standards <a href="https://www.idmp1.com/idmp-standards" rel="noopener noreferrer nofollow">https://www.idmp1.com/idmp-standards</a>] – designed initially for the regulatory scope, but hopefully extensible to other domains – are the most promising solution for solving this known issue, as also highlighted by the <a href="https://unicom-project.eu/" rel="noopener noreferrer nofollow">European project UNICOM</a>. The completion of the IDMP implementation guides, the deployment of the needed supporting services, and the development of some companion standards that will allow the seamless flow of the IDMP identifiers and attributes from the regulatory space to the clinical world (and back) are however still in progress. Additional time is needed before these identifiers and attributes will be available in full for practical use.
Following therefore the IPS principles of “implementability”, “openness" and "extensibility”, the solution proposed here does not rely on IDMP identifiers. Nonetheless, it takes into account, however, relevant IDMP identifiers and attributes which are already usable in the IPS, namely the Pharmaceutical Product Identifiers (PhPIDs), the Medicinal Product Identifier (MPID), and the Medicinal Product Package Identifier (PCID).
Note: IDMP Medicinal Product (MPID) and Medicinal Product Package (PCID) identifiers depend on the market authorization. The “same” product might therefore have different IDs if different authorizations have been received in different countries, while the PhPID should be the same. For the purpose of the IPS, future standards and implementation guides should define global product identifiers that do not depend on the drug registration process (as the Virtual Medicinal Product in SNOMED CT) and relate to IDMP identifiers.
Thus, in the absence of a global identification system for medicinal products, the solution proposed here is based on the approach initially adopted by the European cross-border services (epSOS and currently by the eHDSI project), reused by the IHE Pharmacy templates and more recently adopted (for specific cases) by the HL7 Pharmacy Medication statement templates. The main idea is to integrate local drug identifiers (e.g. product codes) with all the relevant identifying and descriptive attributes that may help the receiver to understand the type of product the sender is referring to, e.g.: active ingredients, administrative dose forms, strength, route of administration and package description.
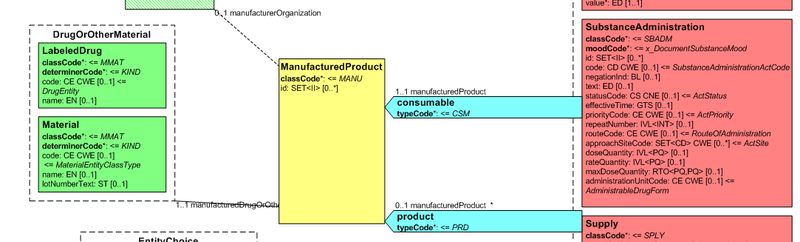
Medication data is usually represented in the CDA Templates using the manufacturedMaterial class, which includes a code and a name to describe any level of the product: packaged product, medicinal product, classes or clusters or products, and so on.
This information is not however sufficient for covering the requirements of the IPS.
Figure: Representation of medicines in CDA
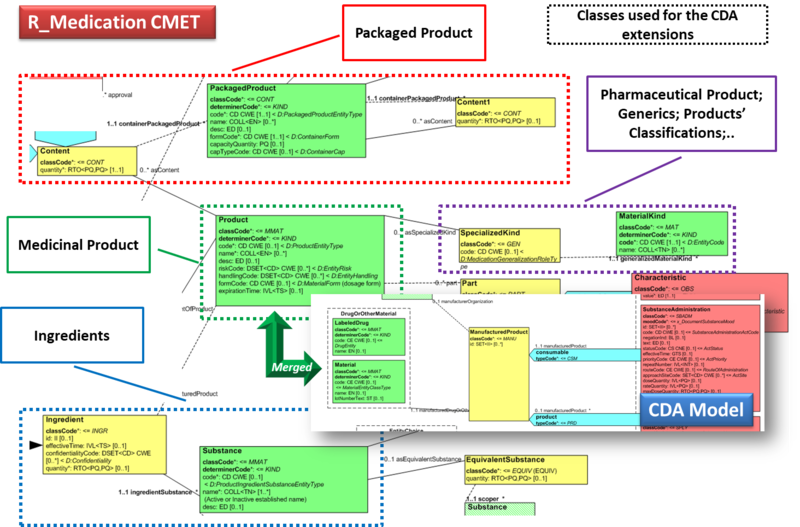
Hence, in order to describe these attributes the CDA model has been extended enhancing the Manufactured Material class with attributes and relationships derived from the latest published version of the R_Medication CMET based on the HL7 Common Product Model (“The common product model is used to improve the alignment between the different representations of products used within the body of HL7 Version 3 models. One goal of this effort is to make it possible to have a single representation, which could then be used as a common message element type (CMET) across those models.”) .
The next figure provides an overview of the CDA model extensions, approach adopted and further developed by the HL7 CDA® R2 Implementation Guide: Pharmacy Templates.
Starting from this IG version, the HL7 CDA IPS medication templates have been defined as specialization of the Pharmacy ones, adopting the pharm (urn:hl7-org:pharm) extensions.
Figure: Extension of the CDA model from the content of the R_Medication CMET.
Conformance clause
This section references the requirements, criteria, or conditions to be satisfied in order that a product (tangible) or a service may claim conformance to this guide, and how other artifacts may claim compliance with it. (Note: The concept of conformance and compliance are used coherently with the HL7 Service-Aware Interoperability Framework: Canonical Definition Specification, Release 2 [HL7 Service-Aware Interoperability Framework: Canonical Definition Specification, Release 2 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=3].
The fulfilment of these clauses indirectly assures that a product that is the subject of a “conformity assessment” satisfies the business or the design requirements this specification complies to. It should, however, be clear that compliance with the specified business or design requirements, for example with the EN ISO 17269 IPS, does not imply that the compliant implementations are technically interoperable.
A “conformity assessment” is a process that assesses that any proposition that is true in a given specification is also true in the service or product that implements it. In most real-world cases conformance testing objects are used to technically validate the products. These objects provide a great help in the validation of the instances, even if they are most often not sufficient to guarantee the functional/ semantic conformity: many real-life examples can be made about instances that are technically valid, but not clinically meaningful or correct.
The "rules" and processes for refining the standard through constraint and extension, including which standard artifacts are subject to constraint or extension; the definition of constraint and localization profiles; the criteria for establishing a conformance statement; and the principles guiding who may define extensions to the standards and under what circumstances they apply to the CDA standards are defined in §1.3 CDA Conformance of the CDA and detailed in the HL7 V3 Refinement, Constraint and Localization section (see the CDA R2 Standard [CDA R2 Standard]).
This guide does not provide additional requirements regarding the Recipient and the Originator Responsibilities.
The formal representation used in this implementation guide for expressing the conformance statement is described in chapter "How to read the table view for templates" of this guide and makes use of a tabular representation that may include also computable or textual constraints. The template rules are formalized using the computable format defined by the HL7 Templates Standard: Specification and Use of Reusable Information Constraint Templates, Release 1 [HL7 Templates Standard: Specification and Use of Reusable Information Constraint Templates, Release 1 http://www.hl7.org/implement/standards/product_brief.cfm?product_id=377] in order to facilitate also the automatic generation of consistent testing and validation capabilities.
The HL7 Templates Standard: "Specification and Use of Reusable Information Constraint Templates, Release 1" defines also how derived templates may relate to the templates defined in this guide for example:
- Specialization: “A specialized template is a narrower, more explicit, more constrained template based on a “parent” template.
- Adaptation: “The adapted template is “based on” the original template which means it can be an extension or a specialization (restriction) of the original template design.”
- Equivalency: “two templates have the same purpose and the same design; however, their governance and/or metadata and/or details of their design may be different.”
Based on this the following way to use this guide may be considered :
- IPS as a document: the conformance is asserted at the document level. All the rules defined by this guide, or by a specialized IPS document level template, are fulfilled. Implementers may take advantage of the template openness to better support specific cases - “extended” parts, however, may not be interoperable among them.
- IPS as a library: the conformance is asserted at the section or the entry level. The templates are used as a library to build, for example, new cross-border documents. For example the immunization section may be used to build an electronic implementation of the WHO yellow card for vaccinations; or the IPS section templates are used to communicate to the country of affiliation minimal and non-exhaustive information about the encounter in which the Patient Summary has been used (cross-border encounter report ). Implementers may take advantage of the template openness to better support specific cases - "extended” parts, however, may not be interoperable among them.
- IPS as a reference: the implementation is conformant with templates that are an adaptation of or equivalent to those defined by this guide. In this case some of the rules defined by this guide are not fulfilled and the conformance cannot be asserted. However, differences may be limited and the effort required to achieve the harmonization may not be not large. Typical examples are templates in which alternatives vocabularies are used.
Jurisdictions may also decide to impose the closure of the template in order to limit the implementation optionality.
This should be carefully evaluated in terms of the flexibility of the solution.
Appendix (Informative)
Acronyms and abbreviations
-
CCD: Continuity of Care Document
-
C-CDA: Consolidated CDA
-
CDA: Clinical Document Architecture
-
CEN: Comité Européen de Normalisation (European Committee for Standardization)
-
CEN/TC 251 : CEN Technical Committe 251
-
DSTU: Draft Standard for Trial Use
-
EC: European Commission
-
EDQM: European Directorate for the Quality of Medicines & Healthcare
-
eHDSI: Digital Service Infrastructure for eHealth
-
eHN: eHealth Network
-
EHR: Electronic Healthcare Record
-
EN: European Normative [or Standard] (CEN)
-
epSOS: European Patient Smart Open Services
-
EU: European; Europe
-
FDA: Food and Drug Administration (USA)
-
GP: General Practitioner
-
HL7: Health Level Seven
-
HP: Healthcare Professional
-
IDMP: IDentification of Medicinal Products (ISO Standard)
-
IHE: Integrating the Healthcare Enterprise
-
INTERPAS: International Patient Summary (HL7 International Project)
-
IPS: International Patient Summary
-
ISO: International Organization for Standardization
-
JAseHN: Joint Action to Support the eHealth Network
-
JIC: Joint Initiative Council on SDO Global Health Informatics Standardization
-
LOINC: Logical Observation Identifiers Names & Codes
-
MOU: Memorandum of Understanding (on cooperation surrounding health related information and communication technologies, that between EU and US)
-
MPID: Medicinal Product Identifier
-
ONC: Office of the National Coordinator for Health Information Technology (USA)
-
PCC: Patient Care Coordination
-
PCID : Medicinal Product Package Identifier
-
PhPID(s): Pharmaceutical Product Identifier(s)
-
prEN: Draft European Normative [or Standard] (CEN)
-
prTS: Draft Technical Specifications (CEN)
-
PS: Patient Summary
-
S&I: Standards and Interoperability (S&I) Framework (run by ONC)
-
SAIF: Service Aware Interoperability Framework
-
SDO: Standards Developing Organization
-
STU: Standard for Trial Use
-
TS: Technical Specifications (CEN)
-
UCUM: Unified Code for Units of Measure
-
WHO: World Health Organization
Glossary
-
Compliance. A standard or specification is compliant with another standard or specification if all propositions that are true in the initial standard are also true in the complying standard. The target artifact is compliant with the source artifact if and only if all conforming implementations of the target are also conforming with the source (RM-ODP). The term compliance is also used to state expectations as to how certain specifications need to satisfy possible legislative or regulatory constraints or requirements.
-
Conformance relates an implementation to a standard. Any proposition that is true of the specification must be true in its implementation. (ISO, 2010).
-
Conformance Assessment is a process whereby a given implementation instance is evaluated to determine which of its various Conformance Assertions are valid implementations of a given specification’s Conformance Statements.
-
Conformance Statement is a statement that identifies testable requirements at a specified Conformance Point within a specification, explicitly defining the behavior which must be satisfied at these points. Conformance Statements will only occur in standard which are intended to constrain some feature of a real implementation, so that there exists, in principle, the possibility of testing.
-
Conformance Assertion is a testable, verifiable statement made about a specific implementation instance against a corresponding Conformance Statement.
-
Conformance Points are the evaluation of conformance at specific points in the implementation or specification. See Conformance.
-
Electronic Patient Summary: electronic health record extract containing essential healthcare information intended for specific uses . (EN ISO 13940: 2016)
-
International Patient Summary : electronic patient summary for use in the unscheduled, cross-border care scenario comprising at least the required elements of the IPS dataset.
-
International Patient Summary dataset: a minimal and non-exhaustive patient summary dataset, specialty-agnostic, condition-independent, but readily usable by clinicians for the cross-border unscheduled care of a patient.
Real World User Stories
This section reports a series of real world user stories adapted from the Trillium Bridge project [The Trillium Bridge Project http://www.trilliumbridge.eu] and the eHDSI initiative [The eHDSI initiative https://ec.europa.eu/cefdigital/wiki/display/EHOPERATIONS/eHealth+DSI+Operations+Home].
IPS Storyboard 1: Martha, a traveling corporate executive
Martha, a 45-year old corporate executive and breast cancer survivor travels frequently on business between the US and EU countries. She carries a clinical summary on her mobile phone and on paper just in case she needs to seek medical care regarding recurring symptoms. Martha’s summary includes
-
Breast cancer Stage II with no evidence of recurrence following treatment
-
hot flashes as problems
-
Anastrozole 1 mg. once daily
-
Black Cohosh Extract herbal supplement as medications
-
the indication of an allergy to Penicillin
-
and finally as Plan of Care, to continue hormone medication with Anastrozole for total of 5 years
-
and monitor for potential breast cancer recurrence.
During a visit in Austria, Martha walks up a hill and experiences shortness of breath, faints, and wakes up a few minutes later after hitting her head on a stone step. A passerby helps her get to the emergency department of a local hospital. An ambulance is called and she is brought to the emergency ward.
During registration and admission, Martha hands in her patient summary in a USB key. At the hospital, Martha is evaluated by an oncologist and a cardiologist.
Following care provision, Martha receives an encounter report. When back home she hands in the encounter report to her primary physician, who updates her record.
IPS Storyboard 2: Paolo, a retired businessman
Paolo Cerruti is a 67-year-old retired businessman, who normally lives in the outskirts Bergamo, near Lake Como, in Lombardy. He is generally healthy, but has long-standing hypertension. His regular physician changed his medication two weeks ago because of poor blood pressure control on his previous medication. He is on holiday going through New England, US, travelling on his own to enjoy the autumn foliage, and is presently in Boston, MA. He is nearing the end of his holiday, and will be returning to Italy in three days’ time. Two days ago he lost his day bag. The bag included his hypertension medication, and he has not been able to take his tablets for two days.
This morning he has woken up feeling dizzy and has blurred vision. The hotel is able to put him in urgent contact with a local general practitioner (GP). Having assessed him, the GP noted a raised blood pressure, but is uncertain about whether to attribute these symptoms to the raised blood pressure or a side effect of the new medication. Now, the GP in Boston needs to know the medication, and the past few blood pressure readings to determine how exceptional the present reading is and manage Paolo appropriately.
Immediate access to his International Patient Summary would be the perfect answer. Paolo may retrieve his online European Patient Summary for emergency access that is retrieved, transformed into an IPS and shown its content translated in English.
The GP notes that visual disturbances are a recognized side effect of this medication. No specific treatment is indicated, and Paolo is reassured that side effects will gradually subside, and his GP can prescribe a suitable antihypertensive medication upon his return to Lake Como.
IPS Storyboard 3: Diana, a pregnant woman
Diana is a 34-year-old pregnant woman from Lisbon with a past medical history of allergic asthma and thyroid cancer during adolescence; for the latter she had a surgical procedure done (thyroidectomy) and, as a consequence, suffers hypothyroidism which requires hormone replacement for life (levothyroxine). At the age of 31 she was diagnosed with a hereditary cardiac disorder – Brugada Syndrome – and had a cardioverter defibrillator implanted to control potentially lethal arrhythmias.
During the pregnancy of her first child (C-section delivery), she suffered gestational diabetes that developed into type 2 diabetes after giving birth and needs now to receive subcutaneous insulin. As chronic treatment she also needs nebulizations three-time per day for her asthma - this condition is aggravated in her case by being a smoker (1 pack per day) as included in the Social History Section.
At this moment, she presents severe pre-eclampsia (hypertension during pregnancy) in treatment with two oral antihypertensive agents (a combination medication). Additionally, she is following a 14-day-course of antibiotic treatment due to an acute pyelonephritis (kidney infection more likely to be develop in pregnant women due to the physiological changes that may interfere with the flow of urine).
Other sections of her Summary include allergies to latex and kiwi (which are very often associated) and to aspirin, and intolerance to lactose; immunizations administered during childhood and adolescence are also present.
Although being real choices for the different diseases and conditions, the selection of the patient's current medication tries to present some easily described medication as well as not so easily ones: e.g. insulin degludec, amoxicilin+clavulanic acid, and the combination of ipratropium bromide+salbutamol for nebulization. For the oral treatment of the pre-eclampsia the agents selected would not be used in real practice during pregnancy.
Integrated examples
The IPS specification releases are published at hl7intl.art-decor.org the International Patient Summary Project Publication Page [International Patient Summary Project Publication Page https://hl7intl.art-decor.pub/index.php?prefix=hl7ips-]. The actual release has a link to the XML materials that the W3C schemas are part of; it also includes example CDA document instances. A set of use cases have been defined and represented in IPS format. Also multiple languages are covered.
It is likely that the publication site will move to hl7.org permanently, and we will inform the community about that process.
Validation artifacts
You can test your implementation (instances) against the IPS specification. To download materials to your computer for local testing and validation consider...
-
...the W3C schemas (actually valid for any CDA specification) located at the Publication Page [https://hl7intl.art-decor.pub/index.php?prefix=hl7ips-]. The actual release has a link to the XML materials as which the W3C schemas are part of; it also includes example CDA document instances.
-
..the ISO schematron, automatically generated by the tool. These are files to do validation locally by associating IPS CDA instances with the main schematron using an XML editor or to use the derived XSLT conversions and apply the according XSLT derivation to your local IPS CDA instance.
For further information you can follow the documentation.
Operational information
-
The IPS project has an official mailing list address ips(at)lists.hl7.org, hosted at the HL7 listserver. Visit your Listserv Subscriptions at hl7.org and subscribe to the International Patient Summary (IPS)that is summarised under the Structured Documents Work Group.
-
The original specification is hosted on the logical ART-DECOR main server art-decor.org under the Governance Group HL7 International, the project is reachable at the Live Project Landing Page.
-
Any IPS specification release in HTML format resides at the Publication Page [https://hl7intl.art-decor.pub/index.php?prefix=hl7ips-]. It is likely that the publication site will move to hl7.org permanently, we will inform about that process.
-
The IPS specification on the wiki is hosted here (international-patient-summary.net). It is likely that the publication site will move to hl7.org permanently, we will inform about that process.
Licenses
Following is a non-exhaustive list of third-party terminologies that may require a separate license:
-
SNOMED CT: SNOMED International (formerly know as International Healthcare Terminology Standards Development Organization IHTSDO, see Get SNOMED CT http://www.ihtsdo.org/snomed-ct/get-snomed-ct) or info@ihtsdo.org
-
Logical Observation Identifiers Names & Codes (LOINC): This material contains content from LOINC® (http://loinc.org). The LOINC Table, LOINC Table Core, LOINC Panels and Forms File, LOINC Answer File, LOINC Part File, LOINC Group File, LOINC Document Ontology File, LOINC Hierarchies, LOINC Linguistic Variants File, LOINC/RSNA Radiology Playbook, and LOINC/IEEE Medical Device Code Mapping Table are copyright © 1995-2017, Regenstrief Institute, Inc. and the Logical Observation Identifiers Names and Codes (LOINC) Committee and is available at no cost under the license at http://loinc.org/license.
-
Unified Code for Units of Measure (UCUM) : Regenstrief Institute, Inc. and the UCUM Organization
-
EDQM Standard Terms : European Directorate for the Quality of Medicines & Healthcare (EDQM, see EDQM Standard Terms https://standardterms.edqm.eu).
FAQ’s
This is a placeholder for future Frequently Asked Questions about the International Patient Summary.